we always provide the food and water needed
We always provide those for whom we care with the basic needs they require – they are kept clean, warm and dry; provided with clothing and shelter; and given food and water. These are fundamental human responses to our neighbor in need. Like the Good Samaritan, we provide each of these things for all whom we encounter.
In the context of nutrition and hydration, the key question is … “What does this person need – in terms of food and water – and how can we best provide this?”
unique needs at the end-of-life
In the same way that a person at the beginning of life needs her food and water provided in a unique manner (indeed a very unique manner the first nine months of her existence), the person nearing the end of life has unique needs. She tends to be more comfortable with smaller amounts of cool/cold/frozen liquids given more frequently (than three times a day). Family members and friends at the bedside of their loved one, if taught a few basic techniques and given a few simple utensils are more than capable of providing the nutrition and hydration the dying person needs.
As persons enter the dying process it is very normal for them to eat and drink less – their bodies are much less active and their body systems are shutting down and therefore the body has less need for calories and fluids. Indeed in the very last few days of life, their food and water needs may be satisfied with the hydration they receive via the frequent oral care provided by caregivers (i.e. frequently soaking a (swab) in water or other liquid the person seems to like and moistening their oral mucosa).
our best guide is comfort and enjoyment
Our best guide to the appropriate amount of food and water is the person’s enjoyment and comfort. Again, much like a parent feeding their baby, a sensitive caregiver, if given some basic guidance/instruction, will be more than capable of gauging these responses.
wrong ways to ask the question
We do not want to fall in the trap of asking questions like …“Should we give food and water to this person?” or “Should we start/stop a feeding tube?” Framing our approach in this way assumes that there are situations in which we would not provide those for whom we care with the basic needs they require. Just as we always have need for warmth and cleanliness and shelter, so also we always have need for food and water. The question is how much and in what manner.
common misconceptions of doctors and nurses
The dying process is often not recognized by the medical professionals caring for the person and consequently the person is given the amount and volume of nutrition and hydration as would be given to someone in a curative situation. There are a number of reasons this may take place including the physician not having been trained in the recognition and ‘diagnosis’ of the dying person, denial of the fact that ‘my’ patient could be dying, unrealistic hope that the dying process can be reversed with appropriate nutrition and hydration, (mis)application of formulas designed to calculate appropriate amounts of nutrition and hydration for younger, healthier persons, acquiescing to family demands as well as other reasons.
common misconceptions of family and friends
Often the person is given too much to eat and drink by well intentioned family members. This may be done because of a lack of understanding of nutritional needs in the dying process, a feeling of a need to “do something”, long standing cultural norms that equate provision of food and drink with love & hospitality, as well as the feeling of a moral imperative that to do anything else would be “starving the person to death”.
consequences of too much food and water
When the dying person receives an excess amount of food and water there are several consequences that may ensue. In general, these are similar to how any of us would feel when we eat and drink too much. The person feels bloated, nauseous, and swollen. The person may have diarrhea because of the inability of the gastrointestinal tract to absorb all that is being put into it. All the extra fluid may pool in the lungs and cause difficulty breathing and shortness of breath. The contents of the stomach may back up and regurgitate and cause heartburn, aspiration (stomach contents going in to the lungs), cough and vomiting.
common concerns – ‘starving’, suffering, ‘killing’
Three common concerns are … being “starved” to death, pain and suffering, and we are “killing” the patient. These are inter-related and addressed in the discussion above.
As the person enters the dying process, they naturally take in less food and water – but it is the appropriate amount for them given their current situation. In contrast, starving someone to death is when we give them inadequate food and water for their needs. This is not what is happening.
This whole process has been studied in a variety of settings and the experience of many doctors and nurses who work in hospice and palliative medicine attest that the person does not experience pain and suffering – when their needs are appropriately addressed. Indeed, the best guide to the person’s food and water needs is precisely their comfort. We have seen much more pain and suffering inflicted by forcing too much food and water into the person, than by them not receiving enough.
Given all of this, it is clear that we are not killing the patient, that the patient’s death is not being hastened because of a lack of food and water. Again, in our experience, the contrary is the case, i.e. excess food and water contributes to conditions that make the person sicker and may well hasten their death (aspiration pneumonia, heart failure, etc.)
the severely disabled
A significant concern is for those who are severely disabled – dementia, stroke, “vegetative” state – but not actively dying. We will best meet their needs by again asking the same question … not “Should we put in a feeding tube?” … but … “What are their food and water needs and how can we best provide for this?” Each person will be different. There are now many studies showing that feeding tubes do not necessarily help and may in fact cause harm. In general, gentle hand feeding is best – loving, attentive caregivers who individualize care to this specific person – again, much like a mother and her baby.
coda
We might consider “the death of St. Francis, who refused “extraordinary” treatment from his doctors and had stopped eating. However, Lady Jacoba, his friend, had come from Rome with his favorite almond cookies. He ate little bits of these cookies from her hand before he died. Perhaps it was a foretaste of what we are all promised in Christ Jesus.” (my thanks to my Franciscan physician friend Dan Sulmasy for this anecdote.)
life phases
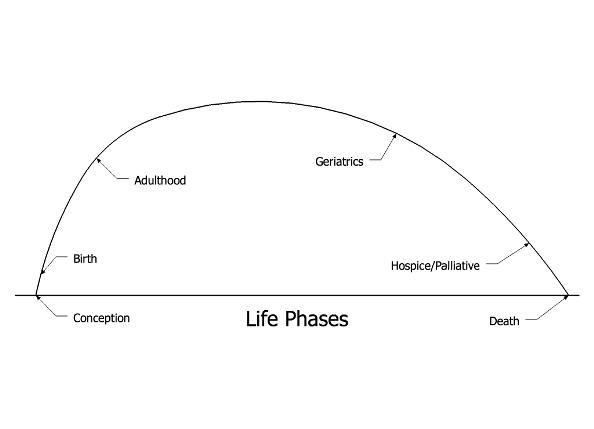
We all tend to project our needs, wants and desires onto those around us. So too with food and water needs. The figure below is intended to illustrate this.
We are trained and have experience with the food and water needs of adults. Whether the doctor trained to use a feeding tube or the spouse ‘trained’ to serve a hamburger and fries, we project this experience onto those at the end of life. But this does not address their needs – which have changed. It would be like trying to feed a burger and fries to a newborn infant – this is not where their body is ‘at’. So, as discussed above, we must adjust to the patient’s true needs.
Pingback: dying in community …
Pingback: food & water based on patient need …